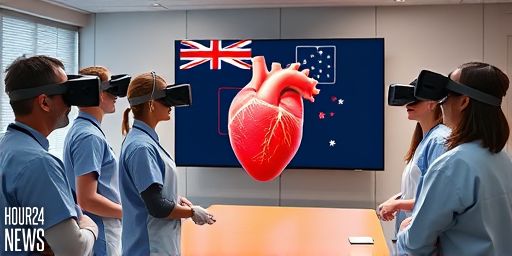
Revolutionizing pediatric heart care with immersive tech
In a groundbreaking collaboration, surgeons at Perth Children’s Hospital are stepping into the operating room of the future—before the first incision—using virtual reality (VR) goggles to explore a patient’s heart. This Telethon-funded initiative, a joint effort by Curtin University’s Hub for Immersive Visualisation and eResearch (HIVE) and the hospital, centers on a new mixed reality imaging tool named Minerva. The aim is simple but ambitious: enhance understanding of each child’s unique heart anatomy and plan complex surgeries with greater precision.
Understanding congenital heart disease with a new perspective
Congenital heart disease (CHD) encompasses more than a dozen abnormalities present at birth, affecting heart structures, valves, and major blood vessels. In Australia, about 2,400 to 3,000 babies are born with CHD each year, making it the most common congenital disorder in newborns. Each case can vary significantly in complexity, often presenting multiple challenges in a single patient. For many infants, surgical repairs occur within the first month of life, underscoring the need for meticulous pre-operative planning.
Why VR adds value for surgeons
Traditionally, surgeons rely on imaging studies like CT or MRI scans to map a patient’s heart. But for roughly five percent of cases where anatomy is particularly intricate, traditional images leave room for interpretation. Minerva changes that dynamic by presenting 3D heart anatomy in a mixed-reality environment. Dr. David Andrews, head of cardiothoracic surgery at PCH, explains the advantage: “I can actually walk my way through a heart. I can slice and dice, I can twist and turn, I can go from top, bottom, side, upward, and try and figure out exactly what I’m going to be looking at when I get into surgery.”
The technology behind Minerva
Minerva is the brainchild of Curtin Medical School Professor Zhonghua Sun, a respected figure in medical imaging. The system is designed to be an intuitive, user-friendly VR surgical planner. Curtin HIVE’s Michael Ovens, who developed the software, describes Minerva as the first “easy to use” VR tool that lets clinicians load CT data and then explore it in three dimensions with natural hand movements. “In VR, you can actually see the 3D anatomy how it really exists (in the body),” he notes. The overall goal is to enable surgeons to analyze the mechanical defects, anatomy, and pathology from multiple angles before entering the operating theatre.
Implications for patient safety and outcomes
By enabling a more thorough pre-operative assessment, Minerva aims to reduce intraoperative surprises that can increase risk for tiny hearts and their families. Professor Sun emphasizes that the technology supports developing the optimal surgical approach, which could translate into shorter operative times, fewer complications, and better overall outcomes for children with CHD. While VR adoption in pediatric surgery is not entirely new, applying it to the planning and education of congenital heart disease cases represents a novel frontier with substantial potential.
Beyond planning: broader applications and future rollout
The Minerva platform holds promise beyond just the OR. Its capacity to visualize complex anatomy makes it a powerful teaching tool for junior doctors and a valuable aid in patient-family discussions, helping carers understand the condition and the proposed surgical strategy. In pilot use at Perth Children’s Hospital, clinicians are already exploring how widely the technology can be deployed across cases of varying CHD complexity. The team plans a broader rollout within the next 12 months, bringing VR-based planning into routine use for paediatric cardiac care.
A glimpse into the future of pediatric cardiology
As telethon-funded research drives innovation in imaging and visualization, the frontier of pediatric cardiology appears increasingly hybrid—merging traditional radiology with immersive technology to improve precision and safety. For the families of children with congenital heart disease, Minerva offers a clearer, more collaborative way to prepare for life-saving surgeries. The collaborative model at Curtin and PCH may well serve as a blueprint for other centers seeking to harness virtual reality to enhance surgical planning, education, and patient communication.