Global Guidelines Urge Faster Action to End Postpartum Haemorrhage Deaths
Leading reproductive health organizations have issued landmark guidelines aimed at dramatically reducing deaths from postpartum haemorrhage (PPH). The World Health Organization (WHO), the International Federation of Gynecology and Obstetrics (FIGO), and the International Confederation of Midwives (ICM) released a cohesive set of recommendations that emphasize earlier detection, rapid response, and standardized treatment. The drive behind the guidelines is to prevent tens of thousands of fatalities each year while also reducing long-term health consequences for survivors.
New Diagnostic Criteria for Rapid Action
PPH is a leading cause of maternal mortality worldwide, and many cases occur without obvious risk factors. The guidelines introduce objective diagnostic criteria designed to trigger fast intervention. Notably, clinicians are advised to act when blood loss reaches 300 mL, in addition to monitoring abnormal vital signs—marking a shift from the traditional 500 mL threshold. The guidance also promotes the use of calibrated blood-loss collection drapes to quantify hemorrhage accurately in real time, enabling immediate action when criteria are met.
Immediate Response: The MOTIVE Bundle
Upon diagnosis, health workers are urged to deploy the MOTIVE bundle of actions without delay. This structured approach includes:
- Massage of the uterus
- Administration of oxytocic drugs to stimulate uterine contractions
- Use of tranexamic acid (TXA) to reduce bleeding
- Intravenous fluids to stabilize circulation
- Vaginal and genital tract examination to assess ongoing bleeding
- Escalation of care if bleeding persists
In rare cases where bleeding continues, the guidelines support additional interventions such as surgery or blood transfusion to stabilize the patient while longer-term treatment is arranged. The overarching aim is to ensure that PPH is recognized early and treated effectively across diverse healthcare settings.
Prevention: Strengthening Antenatal and Postnatal Care
The guidelines also stress prevention by improving maternal health before, during, and after delivery. A key focus is reducing anaemia, which increases the risk of PPH and worsens outcomes when it occurs. Recommendations include daily oral iron and folate during pregnancy, with intravenous iron transfusions when rapid correction is needed, including after PPH events. When appropriate, misoprostol remains a last-resort option where other uterotonics are not available or the cold chain is unreliable.
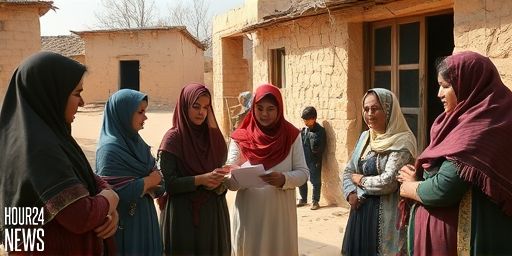
Role of Midwives and Health Systems
Midwives and frontline health workers are central to the guidelines’ success. They are empowered with practical tools and training to recognize early warning signs, administer life-saving interventions, and escalate care swiftly. As ICM President Professor Jacqueline Dunkley-Bent emphasized, governments and donors must invest in maternal care and the workforce, particularly midwives, to turn these guidelines into real-world reductions in PPH deaths.
Resources to Support Implementation
To accompany the 51 recommendations, a suite of training and implementation resources has been developed with partners including UNFPA. Practical modules support frontline workers, national-level adoption plans guide policy changes, and simulation-based training strengthens emergency response capabilities. The guidelines form a critical component of the Global Roadmap to Combat Postpartum Haemorrhage (2023–2030), launched at the 2025 FIGO World Congress in Cape Town, South Africa.
Context and Impact
Publishing the guidelines simultaneously with new research on diagnostic accuracy—based on more than 300,000 women across 23 countries—highlights the commitment to evidence-based practice. The Lancet study reinforces the value of early detection indicators in predicting severe morbidity and maternal mortality, reinforcing the need for widespread adoption of the revised diagnostic thresholds and treatment protocols.
Looking Ahead
With backing from major health institutions and philanthropic support, the guidelines aim to reduce PPH deaths and minimize long-term harm for survivors. As Dr. Jeremy Farrar notes, the recommendations are designed to maximize impact where resources are limited, ensuring more women survive childbirth and return home to their families.