Introduction: Why housing matters in dengue dynamics
Dengue fever continues to pose a significant public health challenge in Malaysia, particularly in districts undergoing rapid urbanization. Beyond mosquito biology, the layout and quality of housing can influence where Aedes aegypti mosquitoes breed, rest, and bite. As cities expand, the way homes are built, organized, and serviced becomes a key, often overlooked, driver of dengue transmission. This article synthesizes recent geospatial and environmental findings to explain how housing structure shapes dengue risk in fast-growing Malaysian districts.
Linking housing design to mosquito behavior
Aedes aegypti thrives in human-made environments. Small differences in housing—such as window screens, wall materials, open eaves, and water storage practices—can alter mosquito resting sites and breeding opportunities. In compact, new urban developments with dense housing blocks, humidity levels and microclimates can encourage mosquito survivorship. Traditional or poorly maintained housing with exposed water containers increases larval habitats, while modern dwellings with secure barriers often reduce exposure. Studies highlight that the intersection of indoor environments and peri-domestic spaces is crucial for transmission dynamics.
Geospatial perspectives: mapping risk to housing types
Recent GIS-based analyses in Malaysia have demonstrated that dengue density correlates with housing characteristics in urbanizing districts. By overlaying geospatial layers of housing age, building materials, and municipal services with dengue case data, researchers can identify hotspots linked to specific housing patterns. For example, areas with older, poorly maintained housing may show higher vector densities due to stagnant water in containers and cracked walls, while newer, well-planned neighborhoods with proper waste management may exhibit lower transmission potential. These insights help public health authorities target vector control where it matters most.
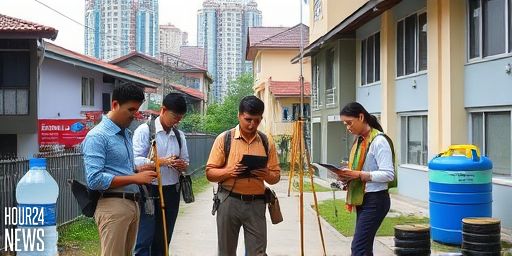
Case in point: Kuantan and comparable districts
Geospatial studies in Kuantan, Malaysia, illustrate how housing structure interacts with urban expansion to shape dengue risk. As districts modernize, informal settlements and older housing stock often persist at the urban fringes. The resulting heterogeneity creates a mosaic of transmission risk, where some neighborhoods experience higher mosquito density and human–mosquito contact. The take-home message is that urban planning and housing policy should integrate vector-control considerations alongside infrastructure development.
Environmental and anthropic factors beyond housing
While housing quality is pivotal, dengue dynamics also reflect environmental and human behaviors. Rainfall patterns, waste management, water storage practices, and community participation in vector control all shape outcomes. The interaction between housing structure and these factors means interventions must be multifaceted: improving housing barriers, promoting rational water storage, and fostering neighborhood clean-up efforts. A comprehensive approach reduces breeding sites while limiting mosquito-human contact, especially in growing districts where population density rises quickly.
Policy implications: designing healthier, dengue-resilient neighborhoods
Public health planning should partner with urban developers, housing authorities, and local communities. Policy recommendations include:
– Incentivizing vector-proof housing features (e.g., intact screens, secure doors, sealed drainage).
– Ensuring reliable water and waste services to reduce home-based breeding sites.
– Prioritizing vector-control resources in areas identified by geospatial analyses as housing-related hotspots.
– Engaging residents in educational programs that emphasize household-level prevention and timely reporting of cases.
These strategies can help Malaysia’s rapidly urbanizing districts curb dengue transmission, even as cities expand and evolve.
Conclusion: housing as a lever in dengue control
Housing structure is more than a shelter—it is a determinant of dengue transmission dynamics in fast-growing Malaysian districts. By integrating housing data with geospatial tools, health authorities can map risk, allocate resources efficiently, and design neighborhoods that reduce vector habitats. As urbanization continues, aligning housing policy with infectious-disease control will be essential to safeguarding public health.