Understanding Dengue in a Rapidly Urbanizing Malaysia
As Malaysia’s urban areas swell in the face of population growth and development, public health officials are paying closer attention to how the built environment influences dengue transmission. A growing body of research suggests that the design and arrangement of housing, as well as nearby infrastructure, can shape the movements and breeding opportunities of the Aedes mosquito—primarily Aedes aegypti—the species responsible for most dengue outbreaks. In a rapidly urbanizing district in Malaysia, researchers have started to map how housing structure interacts with water storage, waste management, and human behavior to drive dengue risk.
Housing Structure as a Key Driver
Traditional housing layouts—core courtyards, close-knit neighborhoods, and compact plots—create microenvironments that influence mosquito life cycles. In districts undergoing fast urbanization, new housing blocks often replace more permeable spaces with dense, multi-story structures and asphalt-heavy landscapes. These changes can reduce natural drainage and increase the number of artificial water-holding containers, such as water storage jars, discarded tires, and plant pots. Each of these elements offers larvae a resting place and a steady supply of stagnant water, prolonging the mosquito’s breeding season in and around homes.
Conversely, some modern housing designs emphasize improved drainage, sealed rainwater systems, and better waste management. When communities harmonize architectural planning with vector control—incorporating screened windows, covered water containers, and routine waste collection—the frequency and density of Aedes breeding sites decline. The interplay between housing structure and vector ecology becomes particularly evident in districts where urban sprawl meets informal settlements, creating a mosaic of risk profiles within a few kilometers.
Geospatial Insights: Mapping Transmission in the City
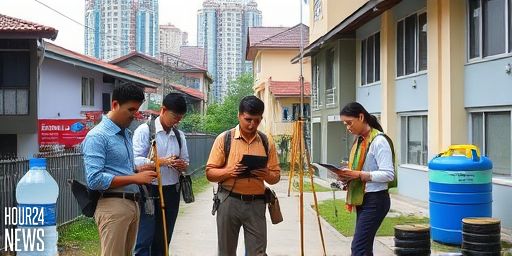
Geospatial analyses, including GIS-based approaches, help public health teams quantify how housing types correlate with dengue density. By overlaying housing maps with mosquito surveillance data, researchers identify hotspots where certain building configurations correlate with higher transmission rates. These maps reveal not only the districts with the most cases but also the housing features that deserve targeted intervention, such as clusters of informal housing lacking reliable water and waste infrastructure.
Spatial models may incorporate variables like plot size, dwelling density, age of housing stock, access to piped water, and proximity to stagnant water sources. When combined with climate data—such as rainfall patterns and temperature—these models produce a nuanced picture of how dengue risk evolves over the monsoon season and into the dry spell. In practice, this means districts can prioritize vector control resources where housing structure consistently aligns with transmission hot spots, rather than deploying broad, one-size-fits-all campaigns.
Implications for Public Health Policy
The link between housing design and dengue dynamics carries direct implications for policy. Urban planners, public health officials, and community groups can collaborate to design healthier neighborhoods that deter mosquito breeding while promoting safer living conditions. Some actionable steps include:
- Incorporating mosquito-control features in new housing developments (e.g., screened windows, sealed rainwater tanks).
- Strengthening infrastructure for drainage and waste management in high-density housing clusters.
- Engaging communities in source reduction campaigns tailored to their housing type and daily routines.
- Integrating geospatial dashboards into routine dengue surveillance to rapidly target interventions during peak transmission periods.
In Malaysia’s evolving districts, such evidence-based, place-specific strategies shine a light on why a “one-size-fits-all” approach to dengue control falls short. By prioritizing architectural and infrastructural improvements alongside traditional vector-control measures, districts can reduce mosquito breeding opportunities at the neighborhood scale and slow transmission dynamics across the city.
What This Means for Residents
For residents, the practical takeaway is simple: maintain clean, water-free environments around homes, ensure water-storage containers are tightly closed, and participate in local clean-up campaigns. Yet beyond individual effort, the study emphasizes the need for urban design that minimizes standing water, supports efficient drainage, and ensures consistent garbage collection. When housing structures promote better water management and quiet, well-lit streets, both people and mosquitoes respond—the former with safer living conditions, the latter with fewer breeding opportunities.
Conclusion
As Malaysia continues to urbanize, understanding how housing structure shapes dengue transmission becomes essential to safeguarding public health. The convergence of housing design, geospatial analytics, and community-driven interventions offers a pragmatic path forward: cut breeding sites at the source, leverage data to pinpoint risk, and build healthier neighborhoods that resist dengue outbreaks without sacrificing growth and development.