Understanding the warning signs: Why 85% matters for VPD prevention
Public health officials are sounding the alarm as vaccination coverage for vaccine‑preventable diseases (VPDs) falls below a critical threshold. When immunization rates dip under about 85%, communities become increasingly vulnerable to outbreaks of diseases such as measles, whooping cough (pertussis), diphtheria, and others that vaccines are designed to prevent. A recent report highlights the real risks and the urgent need for targeted action to close gaps in protection.
What the drop means for communities
Vaccine coverage below 85% disrupts herd immunity, a collective shield that protects those who cannot be vaccinated or who do not develop full immunity. When fewer people are immunized, outbreaks can spread more quickly, especially in areas with dense populations, schools, workplaces, and settings where children and older adults gather. Measles, in particular, can transmit rapidly and cause serious illness, hospitalizations, and, in rare cases, death. Other VPDs like pertussis remain persistent threats to infants and vulnerable individuals. The report emphasizes that even short drops in coverage can translate into dozens or hundreds of additional cases over a single season, stretching healthcare systems and diverting resources from other essential services.
Why coverage has declined
Multiple factors contribute to the erosion of vaccination rates. Misinformation and vaccine hesitancy continue to influence perceptions of vaccine safety and necessity. Access barriers—ranging from clinic hours and transportation to costs and misinformation about eligibility—also play a role, particularly in marginalized communities. Political tensions and fragmented health messaging can further complicate efforts to maintain consistent immunization practices. The net effect is a patchwork of high coverage in some areas and pockets of low uptake in others, creating focal points for potential outbreaks.
Protecting communities: practical steps to boost VPD protection
Public health authorities, healthcare providers, schools, employers, and community organizations must collaborate to raise vaccination coverage and reduce outbreak risks. Key actions include:
- Strengthening routine immunization: Ensure eligibility and access for all age groups, with reminders and outreach to families with young children and at-risk adults.
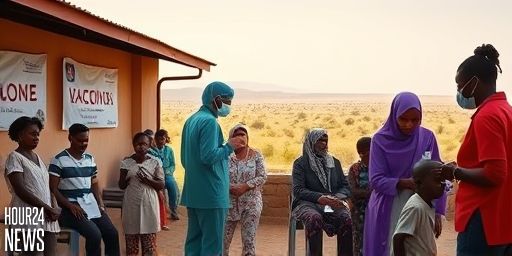
- Catch-up campaigns: Implement targeted campaigns in communities with demonstrated gaps, including school-based clinics and workplace vaccination drives.
- Convenience and access: Extend clinic hours, offer weekend services, and provide mobile vaccination units to reach underserved neighborhoods.
- Clear, science-based communication: Combat misinformation with trusted, transparent messaging about vaccine safety, benefits, and the risks of non-vaccination.
- School and workplace policies: Reinforce immunization requirements for enrollment and employment where appropriate, while offering grace periods and support for those with barriers.
- Data-driven targeting: Use local surveillance to identify outbreak hotspots and direct resources where they’re most needed.
Protecting the most vulnerable
Infants, older adults, pregnant people, and individuals with compromised immune systems are at higher risk for severe outcomes from VPDs. Protecting these groups requires a combination of high community vaccination rates and targeted protections—such as ensuring caregivers and household contacts are up to date with their vaccines. In addition, rapid response capabilities—case investigation, contact tracing, and timely isolation—are essential to contain outbreaks when they occur.
What this means for policy makers and communities
The report underscores that dwindling coverage is not only a health issue but also a policy and equity issue. Investments in public health infrastructure, accurate health communication, and accessible vaccination services pay dividends in reduced disease burden, fewer hospitalizations, and safer schools and workplaces. Policymakers are urged to prioritize funding for immunization programs, remove barriers to access, and support data-sharing systems that help communities monitor coverage in real time.
Takeaway: act now to close the gap
With vaccination coverage slipping below the 85% threshold in parts of the country, the risk of VPD outbreaks looms larger. Proactive, coordinated action can restore protection, prevent needless illness, and safeguard public health. Communities that invest in robust immunization efforts today will reap the benefits of healthier, more resilient populations tomorrow.