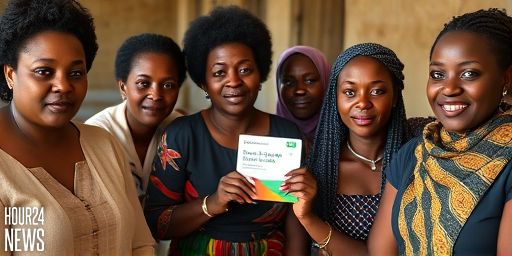
Kenya embraces a new era in cervical cancer screening
In a country where cervical cancer remains a leading cause of cancer-related deaths among women, Kenya is piloting a bold move: HPV self-testing that women can perform at home or in community clinics. The program aims to overcome barriers that have long hindered screening—fear, stigma, distance to clinics, and the cost of professional testing. By enabling women to collect their own samples, health authorities hope to boost participation and catch infections earlier, when treatment is most effective.
Why HPV self-testing matters
Human Papillomavirus is a common infection, and persistent infection with high-risk strains can lead to cervical cancer. Traditional screening methods, such as Pap smears or clinician-collected HPV tests, require a visit to a clinic, trained staff, and follow-up for results. The self-testing approach shifts some of that burden away from health facilities and into communities, giving women more control over their health journey. In settings with limited healthcare resources, self-testing can dramatically increase screening coverage, a critical step toward reducing mortality from cervical cancer.
How the Kenyan program works
The Kenyan initiative involves distributing HPV self-testing kits through primary care facilities, community health workers, and mobile clinics in targeted counties. Women receive clear, multilingual instructions on how to collect a sample, typically from the cervix or a vaginal swab, depending on the kit. After collection, samples are returned to a lab for analysis or, in some models, processed on-site with rapid testing. Results are communicated privately, with counselling and next steps provided for those who test positive for high-risk HPV.
Empowering women with privacy and convenience
One of the strongest appeals of self-testing is privacy—an essential factor in areas where stigma around sexual health can deter women from seeking care. Women can test themselves without exposing personal concerns to family or community members, reducing anxiety and potential social repercussions. Convenience is equally important; the ability to test during weekends or evenings, near home, can remove work and childcare barriers that keep many women from screening.
Impact on early detection and outcomes
Public health experts anticipate that wider adoption of HPV self-testing will lead to earlier detection of high-risk infections, enabling timely follow-up care such as enhanced screening, colposcopy, or treatment where needed. Early-stage cervical cancer is highly curable, and increasing screening uptake is a proven strategy to reduce deaths. The Kenyan health system also uses triage strategies, offering HPV-positive women additional tests to determine the necessity of further procedures, thereby avoiding unnecessary interventions for those at lower risk.
Challenges and considerations
While the promise is substantial, several challenges require attention. Ensuring specimen integrity during transport, maintaining cold chains where necessary, and guaranteeing timely lab results are logistical hurdles. Equity remains a priority: programs must reach rural and low-income populations who may have limited access to health facilities or digital tools. Training health workers, providing culturally sensitive counselling, and ensuring a reliable supply of kits are critical to sustaining momentum.
Policy and community voices
Kenyan health authorities frame HPV self-testing as part of a broader move toward preventive care and universal health coverage. Partnerships with international health organizations, non-governmental groups, and local communities are helping to tailor messaging and distribution to fit local realities. Community health volunteers play a key role in educating women, addressing misconceptions, and guiding those who test positive toward appropriate care pathways.
What this could mean for the future
If the Kenyan model proves effective, it could inspire other low- and middle-income countries to adopt similar self-testing approaches. The potential benefits extend beyond the individual—improved screening rates can lower national cervical cancer incidence and mortality, reducing long-term healthcare costs. As technology and supply chains mature, self-testing could become a standard entry point for preventive cervical health across Africa and beyond.
Closing thoughts
For women like Rachel Adhiambo Odoyo, HPV self-testing represents more than a medical option; it embodies autonomy, reassurance, and a path toward better health for families and communities. The ongoing rollout in Kenya will reveal how this approach can be scaled responsibly, keeping privacy, accuracy, and access at the forefront of cervical cancer prevention.