New Findings Highlight the Power of Lifestyle Interventions in Gestational Diabetes Prevention
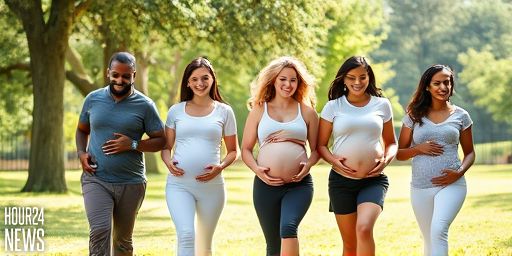
A recent study, co-authored by Professor Fionnuala McAuliffe of the UCD School of Medicine and led by researchers at the University of Liverpool, provides compelling evidence that structured lifestyle interventions can significantly reduce the risk of gestational diabetes mellitus (GDM). The work adds to a growing body of evidence that non-pharmacological strategies can improve maternal and fetal outcomes, offering pregnant individuals practical avenues to safeguard health before and during pregnancy.
Why Gestational Diabetes Matters
Gestational diabetes affects tens of thousands of pregnancies each year and is linked to higher risks of complications such as preeclampsia, cesarean delivery, and future type 2 diabetes for both mother and child. While genetics play a role, lifestyle factors—especially diet, physical activity, and weight management—are modifiable risk drivers. The new research emphasizes that adopting healthier behaviors can be a powerful shield against GDM.
The Intervention: What It Involves
The study evaluated a comprehensive lifestyle program designed for expectant parents. Key components include: balanced nutrition emphasizing whole foods, fiber-rich carbohydrates, and controlled portion sizes; regular, moderate physical activity tailored to pregnancy; and behavioral support to sustain changes. Importantly, the program was accessible, scalable, and adaptable to diverse populations, making it feasible to integrate into standard prenatal care.
Dietary Changes
Nutrition guidance focused on stabilizing blood sugar, improving insulin sensitivity, and preventing excessive gestational weight gain. Emphasis was placed on vegetables, fruit, lean proteins, whole grains, and healthy fats, while limiting refined sugars and highly processed foods. Participants who followed these recommendations showed measurable reductions in GDM incidence compared with those who did not.
Physical Activity
Regular physical activity during pregnancy has well-established benefits for glucose regulation and cardiovascular health. The intervention encouraged safe, moderate-intensity activities—such as walking, swimming, and prenatal yoga—most days of the week. The program also provided guidance on pacing, rest, and recognizing warning signs, ensuring safety for both mother and baby.
Behavioral Support
Lifestyle change is most effective when supported by ongoing motivation and accountability. The study included coaching, goal-setting, and peer support to help pregnant individuals adopt and maintain healthier habits throughout gestation. This holistic approach helped address barriers such as time constraints, fatigue, and cultural food preferences.
Key Findings and Implications
The research demonstrates a meaningful reduction in the risk of gestational diabetes among participants who completed the lifestyle program. Beyond lowering GDM risk, the interventions correlated with healthier birth weights, improved maternal metabolic profiles, and a potential decrease in long-term diabetes risk for offspring. These findings hold promise for public health strategies that prioritize prevention through everyday choices rather than relying solely on medical treatment after diagnosis.
Clinical and Policy Relevance
For clinicians, the study reinforces the value of integrating lifestyle counseling into routine prenatal care. For policymakers, the results support investments in accessible program delivery, including community-based options and digital tools that can reach a wider range of expectant families. Importantly, the research team notes that lifestyle interventions should be culturally sensitive, inclusive, and adaptable to different healthcare settings to maximize impact.
About the Researchers
The work is a collaboration between the University of Liverpool and the UCD School of Medicine, led by researchers including Professor Fionnuala McAuliffe. The cross-institutional effort highlights how combining clinical expertise with public health insights can yield practical, scalable solutions to gestational diabetes risk.
What’s Next?
Future studies aim to refine the intervention components, explore long-term outcomes for mothers and children, and identify which subgroups benefit most. In the meantime, pregnant individuals should speak with their healthcare providers about safe, personalized lifestyle strategies that support healthy pregnancies.