Groundbreaking findings on gestational diabetes prevention
New research co-authored by Professor Fionnuala McAuliffe of the UCD School of Medicine and led by the University of Liverpool provides compelling evidence that lifestyle interventions during pregnancy can significantly reduce the risk of gestational diabetes. This large-scale investigation adds to a growing body of work suggesting that practical, sustainable changes in diet, physical activity, and routine monitoring can influence maternal health outcomes and long-term well-being for both mother and child.
What the study looked at
The study analyzed data from diverse populations, examining how targeted lifestyle strategies impacted the incidence of gestational diabetes mellitus (GDM). Researchers emphasized real-world applicability, focusing on interventions that could be integrated into standard prenatal care without demanding excessive time or resources from patients or clinicians. The key components included nutrition guidance, physical activity plans, and regular glucose screening aligned with contemporary clinical guidelines.
Dietary changes that matter
Dietary interventions centered on balanced macronutrient intake, portion control, and the inclusion of fiber-rich foods. Emphasis was placed on moderating refined carbohydrates and added sugars while ensuring adequate micronutrients essential for pregnancy. Participants who adhered to structured meal planning and mindful eating reported improvements in blood glucose regulation, reduced insulin resistance, and a lower likelihood of developing gestational diabetes.
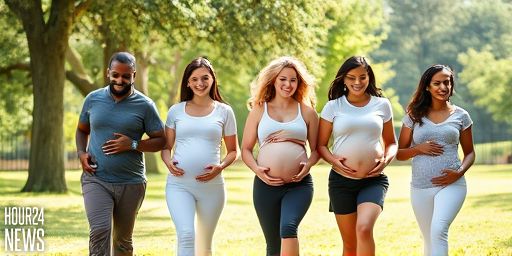
Movement as medicine
Physical activity was another cornerstone of the interventions. The study supports moderate-intensity exercise, such as brisk walking, swimming, or cycling, several times per week, tailored to a person’s fitness level and medical history. Regular activity helps improve glucose uptake by muscles, enhances insulin sensitivity, and can contribute to healthier weight management during pregnancy. Importantly, the program encouraged gradual progression and safety, with professional guidance to minimize risk and maximize adherence.
Monitoring and support mechanisms
Regular monitoring and accessible support were highlighted as critical for success. The research suggests that leveraging routine prenatal visits to include glucose screening, education on recognizing warning signs, and ongoing motivation can bolster adherence to lifestyle changes. Digital tools, peer support groups, and community health workers emerged as effective enablers, helping participants sustain healthy behaviors through pregnancy and beyond.
Why this matters for mothers and babies
Gestational diabetes poses short- and long-term risks for both mother and child, including higher chances of cesarean delivery, macrosomia, and future metabolic conditions. By reducing the incidence of GDM, lifestyle interventions not only support safer pregnancies but may also slow the trajectory toward type 2 diabetes in women who have had gestational diabetes.
Implications for healthcare systems
The study’s implications extend to prenatal care policy and program design. Implementing scalable lifestyle interventions requires a collaborative approach among obstetricians, nutritionists, physical therapists, and primary care providers. Training clinicians to offer brief, actionable counseling and connecting patients with community resources can help integrate these strategies into routine care without overburdening resources.
Practical takeaways for expecting families
Expecting families can translate these findings into concrete steps: adopt a balanced, nutrient-dense diet; aim for regular, safe physical activity aligned with medical advice; seek regular glucose monitoring as recommended by prenatal guidelines; and utilize support networks, digital tools, and community programs to maintain motivation. Small, consistent changes over the course of pregnancy can yield meaningful reductions in gestational diabetes risk and improve overall pregnancy outcomes.
Future directions
Researchers are looking to tailor lifestyle interventions to individual risk profiles, considering factors such as genetics, cultural background, and socioeconomic status. The ongoing work aims to optimize intervention design, ensuring accessibility, cultural relevance, and sustained impact across populations. As evidence grows, healthcare systems may increasingly incorporate structured, scalable lifestyle programs as a standard element of pregnancy care.