New Nanomanufacturing Technique Improves Vascular Networks in Engineered Tissue
Engineered human tissue has long offered a vital bridge between lab discoveries and human clinical trials. A key hurdle, however, has been providing a functional vascular system to sustain cells within three-dimensional constructs. Without adequate blood circulation, large-scale tissue models develop necrotic regions where cells starve for oxygen and nutrients. A recent study from Binghamton University’s Thomas J. Watson College of Engineering and Applied Science proposes a compelling solution: a nanomanufacturing approach that creates micro-scale vascular structures within tissue scaffolds to enhance perfusion and viability.
The Challenge of Building Vascular Networks in 3D Tissue
Our bodies rely on a hierarchical network of vessels—from large arteries down to tiny capillaries—to deliver nutrients and remove waste. Replicating this complexity in vitro has proved difficult. While 3D printing can fabricate larger vessels, the creation of functional microvasculature requires self-assembly and precise material engineering. The research team sought to regulate vessel size and distribution, enabling engineered tissues to maintain viability as they scale up in three dimensions.
Nanomanufacturing as a Solution
The researchers used a combination of two inert polymers, polyethylene oxide (PEO) and polystyrene (PS), to craft microtubes at a remarkably small scale. The process hinges on electrospinning, a technique that uses a strong electric field to form ultra-fine fibers. By forming solid microtubes and subsequently dissolving their cores, the team produced hollow microtubes ranging from 1 to 10 microns in diameter — sizes appropriate for mimicking natural microvasculature. Ultrasonic vibration helped tailor the lengths, ensuring the tubes remained dispersed rather than forming bulky aggregates within the hydrogel medium.
Integrating Microtubes into a Hydrogel Scaffold
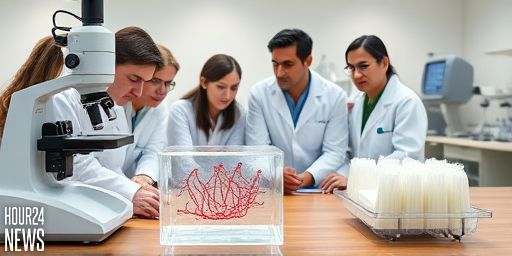
Once fabricated, the hollow microtubes were embedded into a composite hydrogel that serves as the tissue-growing medium. To observe how well these channels support blood flow, researchers introduced fluorescent beads and tracked dispersion through the engineered tissue. The results demonstrated improved distribution of perfusate, indicating enhanced delivery of nutrients and oxygen to cells throughout the construct.
What Makes This Approach Different
Traditional methods often rely on spontaneous self-assembly for microvasculature, which can be unpredictable and poorly controlled. The nanomanufacturing strategy provides a tunable platform for regulating vessel size, spacing, and connectivity. This level of control is essential when attempting to reproduce organ-specific vascular features, such as the blood-brain barrier, which presents unique challenges for tumor studies and neurodegenerative disease research.
Looking Ahead: Toward Organ-Specific Microvasculature
In ongoing work, the team aims to explore how microtube dimensions, shapes, and materials influence vascular outcomes in different tissue contexts. A major goal is to tailor microvasculature to match the demands of specific organs, enabling more physiologically relevant models. By refining this technology, researchers hope to assemble multi-organ living systems from human cells, bringing the physiological relevance of engineered tissues closer to real human biology.
Quotations from the Research Team
“We want to bring the physiological relevance of these engineered tissues closer to our own bodies,” said a faculty member involved in the project. “If we perfect this technology, we can assemble not only a single organ but multiple organs as a living system based on human cells.”
Implications for Biomedical Research and Medicine
Enhanced microvasculature in engineered tissues accelerates preclinical testing, improves data quality, and reduces the risk of necrotic zones that plague larger constructs. Beyond tissue engineering, the ability to tune microvascular networks could advance organ-on-a-chip platforms, tumor biology studies, and therapies targeting barrier tissues such as the blood-brain barrier. As researchers continue to integrate nanomanufactured vascular networks with organ-specific features, the line between engineered tissue and living human tissue may become increasingly blurred in favorable, ethically controlled ways.