VR Brings a New Dimension to Pediatric Heart Surgery
In a bold step forward for congenital heart disease care, paediatric heart surgeons are donning virtual reality (VR) goggles to step inside the hearts of their tiniest patients. The Minerva project, a collaboration between Curtin University’s Hub for Immersive Visualisation and eResearch (HIVE) and Perth Children’s Hospital, is redefining how teams prepare for complex surgeries in newborns and infants.
From Traditional Imaging to Immersive Planning
Congenital heart disease (CHD) encompasses more than a dozen abnormalities affecting the heart, valves, or major blood vessels present at birth. Each case presents unique challenges, and for Australian babies, CHD remains the most common congenital disorder. With 2,400 to 3,000 new cases annually, surgeons must tailor their approach to the individual anatomy of each patient. As Perth Children’s Hospital head of cardiothoracic surgery Dr. David Andrews notes, “One of the challenges for surgeons is understanding the particular anatomy of each and every patient.”
Traditionally, surgeons rely on imaging modalities such as CT or MRI scans to plan operations. However, for about five percent of CHD cases, the anatomy is so intricate that conventional imaging can fall short of providing a complete spatial understanding before entering the operating room. Minerva changes that by offering a non-invasive, immersive way to “walk through” a patient’s heart.
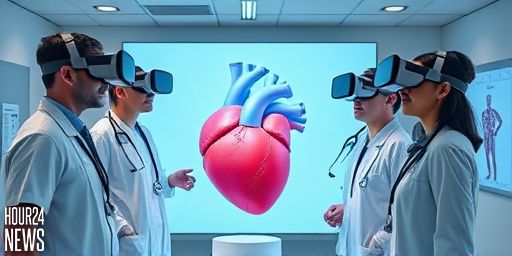
How Minerva Works
Minerva is a mixed-reality imaging tool delivered through VR goggles. Drs. like Andrews can load CT images in real time and explore the virtual heart from any angle—top, bottom, side, or interior—by simply manipulating the data with their hands. Curtin Medical School Professor Zhonghua Sun, the project’s chief investigator, explains the aim: to help paediatric surgeons “develop the optimal surgical approach” and reduce the risks associated with complex surgeries. “You can analyse the mechanical defect, anatomy, pathology from all different angles, so they can have a better understanding about the situation before the surgery,” Professor Sun said.
Real-World Impact and Early Results
Minerva represents a practical, user-friendly step into the future of surgical planning. Curtin HIVE extended reality researcher and developer Michael Ovens describes Minerva as “the first easy to use virtual reality surgical planner.” Surgeons can load imaging data and manipulate it in VR to visualize three-dimensional anatomy as it exists within the body. This enhanced perspective can inform decisions about incision sites, sequence of repairs, and potential intraoperative challenges before the first cut is made.
Clinical Adoption and Education
In pilot use at Perth Children’s Hospital, the Minerva team hopes to expand VR adoption across more clinicians who treat complex CHD cases. The goal is not only to improve surgical planning but also to enhance education and patient communication. VR tools can serve as a powerful teaching aid for junior doctors, streamline clinical workflows, and facilitate clearer discussions with patients’ families about planned procedures and expected outcomes. Professor Sun notes that while VR is not new, applying it to paediatric congenital heart disease in this cohesive, practical way is a novel development with significant promise.
The Telethon Connection and the Path Forward
Funding from a Telethon research grant has made Minerva possible, underscoring the role of philanthropic support in advancing high-impact medical technology. As the team looks ahead to a broader rollout over the next year, the focus will be on validating how VR-assisted planning translates into safer surgeries and better outcomes for children with CHD. For families and clinicians alike, Minerva signals a future where preoperative planning is closer to 4D reality—bringing clarity before small hearts are touched by the knife.
“Virtual reality is not a very new technology,” says Professor Sun, “but in how it could assist with surgical planning of paediatric patients and especially the challenging congenital heart disease, this is a novel area.”