Experts Urge Expanding Meningitis Vaccination to Cover More Strains
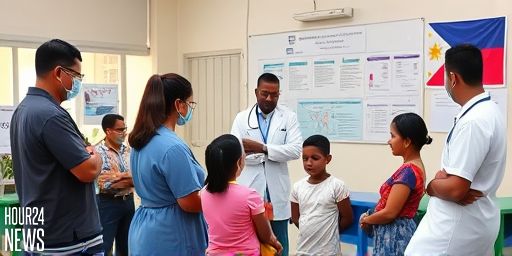
Health professionals in the Philippines are championing broader meningitis vaccination to protect people from a wider range of causative strains. While existing programs target specific bacteria, experts argue that immunity from a single vaccine does not guarantee protection against all meningitis-causing pathogens.
Pediatric neurologist Jo Janette de la Calzada emphasized the need for vaccines that cover multiple invasive strains. “Kaya importante ‘yung vaccine kasi it will cover a lot of the invasive strains na in the hope na hindi talaga siya (individual) matamaan,” she explained, noting that surviving one type of meningitis does not confer immunity against other bacteria or viruses that can cause the disease.
“Pwede talaga, in a sense, kung ibang bacteria na naman. Ibang virus na naman ang [tumama],” de la Calzada added, describing the persistent risk of meningitis recurrence from different pathogens. Pediatric infectious disease specialist Liza Antoinette Gonzales also highlighted a key truth: “You’re not immune to all.”
The call comes as data from the Meningitis Progress Tracker shows the Philippines ranked second among 27 Asia-Pacific countries for meningitis cases in 2021, and 32nd out of 194 countries globally. UNICEF reports that nearly 40% of meningitis-related deaths occur in children under five years old worldwide, underscoring the urgency of more comprehensive vaccination strategies.
Why Broader Coverage Matters
Meningitis can be caused by bacteria, viruses, or fungi, and symptoms—severe headache, seizures, stiff neck, fever, and rashes—often overlap across causes. A vaccine that targets only one strain may leave individuals vulnerable to others, especially in areas with diverse circulating pathogens. The public health takeaway is clear: broader protection could reduce severe outcomes, long-term complications, and the societal burden of disease.
Current Immunization Landscape in the Philippines
At present, the National Immunization Program in the Philippines includes two vaccines: pneumococcal and Haemophilus influenzae vaccines. While these remain critical due to their prevalence, experts warn against over-reliance on a limited set of vaccines when other meningitis-causing organisms continue to circulate.
Gonzales stressed the importance of prioritizing these two vaccines before expanding the meningococcal program. “I would focus maybe to expand the coverage for both of these vaccines first, maybe before introducing the meningococcal vaccine,” she explained. A wider rollout of meningitis vaccines could potentially divert attention from essential cost-effective immunizations already saving lives.
Pathways to Expanded Protection
Efforts to broaden protection include adding Japanese encephalitis and meningococcal vaccines to public health offerings. Private hospitals currently offer these vaccines, but at higher costs, creating inequities in access. Government initiatives to include them in the public health system and the Z Benefit Package under the Philippine Health Insurance Corp are being advocated to improve affordability and uptake.
Public Awareness and Early Action
Public education is a central component of reducing meningitis risk. Health professionals urge people to stay informed about meningitis types and their respective vaccines. Early recognition of symptoms and prompt treatment are crucial, as survivors can face seizures, epilepsy, or neurological and learning difficulties—outcomes that can persist long after the initial illness.
De la Calzada highlighted the long-term consequences: “That’s the problem with meningitis. Kasi you may survive it, but you can have permanent problems. And only time can tell how much you can gain.” The goal is to prevent infections in the first place through smarter vaccination strategies and informed communities.
Role of Institutions and Partnerships
Leading voices from the Philippine Foundation for Vaccination, GSK Philippines, the Philippine Society for Microbiology and Infectious Diseases, and the Pediatric Infectious Disease Society of the Philippines have joined forces to advocate for enhanced meningitis prevention. Their collaboration aims to galvanize policymakers, healthcare providers, and the public to support expanded vaccination, better access, and stronger disease surveillance.
What Comes Next
As the health community weighs the benefits of adding broader meningitis vaccines to public programs, key questions include funding, prioritization, and the logistics of rollout. The consensus is that expanding vaccination coverage—not just of meningitis-specific vaccines but of related immunizations as well—will save lives by reducing incidence, complications, and the long-term burden on families and health systems.
In the words of Gonzales and de la Calzada, continued education, steady surveillance, and strategic vaccine inclusion in public health plans are essential steps toward a future where meningitis is preventable for more people, especially the youngest and most vulnerable.